30yr Female with Fever and Breathlessness
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E-log book also reflects my patient centered online learning portfolio and your valuable inputs on the comment box.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competancy in reading and comprehending clinical data including history, clinical finding, investigations and come up with a diagnosis and treatment plan
CONSENT AND DEIDENTIFICATION :
The patient and the attenders have been adequately informed about this documentation and privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whomsoever.
Upper Respiratory tract examination:
Nostrils- normal
Nasal septum- no deviation
No nasal polyps
No Tonsils
Posterior pharyngeal wall- normal
Lower Respiratory tract examination:
Inspection:
Shape of the chest - Circular
Movement of chest- appears to be equal on both sides
Trachea- appears to be in central position
Apex beat- visible
No scars and sinuses seen
Palpation:
Trachea- Central in position
Apex beat- shifted to left
Increased vocal fremitus
No rib crowding
Percussion:
Right Left
Supra clavicular Resonant Resonant
Clavicular Resonant Resonant
Infra clavicular Resonant Resonant
Mammary Resonant Resonant
Axillary Resonant Resonant
Infra axillary Resonant Resonant
Supar scapular Resonant Resonant
Inter Scapular Resonant Resonant
Infra scapular Resonant. Resonant
Auscultation:
BAE +
Normal vesicular breath sounds
No wheeze
?Tubular sounds in left mammary area
CVS:
S1,S2 heard
No murmurs
CNS :
Upper limb Lower limb
Right Left Right Left
Tone: Normal Normal Normal Normal
Power: 5/5 5/5 5/5 5/5
Reflexes: Right Left
Biceps + +
Triceps + +
Supinator + +
Knee + +
Ankle + +
Plantar Flexion Flexion
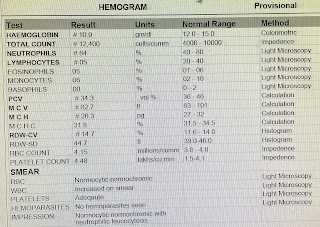
INVESTIGATIONS:
CHEST X-RAY:
ECG:
PROVISIONAL DIAGNOSIS:
Left Upper Lobe Pneumonia with right sided fibrosis;
Pulmonary Koch’s (Sputum-positive for TB)
TREATMENT:
IV Fluids (NS,RL) with Optineuron @75ml/hr
Nebulisation with Duolin 8hrly, Budecort 12hrly
INJ. PIPTAZ 4.5g IV/TID
TAB. AZITHROMYCIN 500mg PO/OD
INJ. PAN 40mg IV/OD BBF
INJ. NEOMOL 1g IV/SOS (if temperature >101F)
TAB. DOLO 650mg PO/SOS
BP,PR,Temperature,RR charting 4hrly.
GRBS charting 6hrly.










Comments
Post a Comment