40yr Female with Fever and Thrombocytopenia
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
PRESENTING COMPLAINTS:
C/O FEVER SINCE 4DAYS,
COLD SINCE 4DAYS,
COUGH WITH SPUTUM SINCE 4DAYS,
GENERALISED BODY PAIN SINCE 3DAYS,
HEADACHE SINCE 3DAYS,
VOMITINGS SINCE 1DAY.
HISTORY OF PRESENTING ILLNESS:
PATIENT WAS APPARENTLY ASYMPTOMATIC 4 DAYS BACK THEN PATIENT DEVELOPED COLD AND FEVER ,HIGH GRADE, INTERMITTENT,ASSOCIATED WITH CHILLS AND RIGOR,RELEIVED ON MEDICATION.
COUGH SINCE 4DAYS ,PRODUCTIVE, WHITE COLOUR, SCANTY AMOUNT
GENERALISED BODY PAINS SINCE 3DAYS AND HEADACHE SINCE 3DAYS, NAUSEA SINCE 1DAY
VOMITINGS SINCE 1DAY 3EPISODES,NON-PROJECTILE,NON-BILIOUS,FOOD AS CONTENT.
NO H/O CHEST PAIN, BURNING MICTURATION,SOB,ABDOMINAL PAIN
NO H/O BLACK COLOURED STOOLS
HISTORY OF PAST ILLNESS:
NOT K/C/O DM,HTN,ASTHMA,CAD
K/C/O TB 10YRS BACK (COMPLETED 6MONTHS COURSE)
PERSONAL HISTORY:
Diet- Mixed
Appetite- DECREASED
Sleep- Adequate
Bowel and Bladder movements- Normal.
GENERAL EXAMINATION:
PATIENT IS CONCIOUS,COHERENT,CO-OPERATIVE
NO PALLOR,ICTERUS, CYANOSIS, CLUBBING, LYMPHADENOPATHY, EDEMA.
TEMPERATURE- 104F
BP- 110/70mmhg
PR- 108bpm
RR- 32cpm
SpO2- 97% AT ROOM AIR
GRBS-222@ ADMISSION
Upper limb Lower limb
Right Left Right Left
Tone: Normal Normal Normal Normal
Power: 5/5 5/5 5/5 5/5
Reflexes: Right Left
Biceps + +
Triceps + +
Supinator + +
Knee + +
Ankle + +
Plantar Flexion Flexion
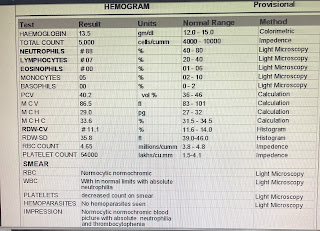
LAB INVESTIGATIONS:
On DAY 1:
On DAY 2:
On DAY 3:
On DAY 4:
On DAY 5:
USG Abdomen:
PROVISIONAL DIAGNOSIS:
Dengue fever (NS1 positive) with Thrombocytopenia.
TREATMENT:
IV fluids NS @100ml/hr
INJ. NEOMOL 1g IV/SOS
TAB. DOLO 650mg PO/TID
TAB. PANTOP 40mg PO/OD
Plenty of oral fluids












Comments
Post a Comment